

Welcome to the Scrambler Therapy® official scientific and clinical information site
On the date this page is being filled, different clinical trials in thousands of cases have been published on different types of severe chronic and oncologic pain resistant to all other treatment. No study has shown any substantial toxicities to the patient.
Considering it is an operator-dependent methodology that calls for an adequate learning curve, the first independent trials show worse outcomes compared to the reference trials. In time, with progress in the methodology knowledge, better training, clinical trials carried out only after having completed the learning curve, and more compliance to standard usage protocols, these differences have progressively decreased or disappeared.
There is still the need for RCTs, but the proper use of ST, that being operator-dependent, allows only for a partial double-blind or single-blind trial design.
Attempts to do a complete double-blind automatically determine substantial changes in the standard treatment protocol. These changes prevent the operator from following the normal procedures registered in the healthcare authorizations and can erase or certainly extremely reduce the efficacy of the treatment, consequently invalidating the scientific data. This methodological problem is present (even more broadly) in many other medically validated treatments, such as, for example, spinal cord stimulator (SCS).
As of today, from a merely scientific viewpoint, to avoid the introduction of added bias that would make the trials unreliable, the solutions could be:
- RCTs vs sham/TENS partially double blind ( ST operator cannot be blind )
- Double-blind with single-arm sham using the same ST device intentionally in the wrong way to analytically determine the placebo effect. The following treatment of the same patients with the normal procedure will guarantee the trial’s ethicality and provide further comparable results. Data from this type of study, the only possible one for a complete double-blind, could later be used in other clinical trials as a virtual control arm, allowing the successful results to have the statistical bias of the placebo effect.
- RCTs vs protocol therapies
Treatment outcome is highly dependent on the operator's ability to correctly identify electrode positioning areas and to fine-tune stimulation intensity. When the procedure is carried out correctly, pain must disappear after the completion of the fine-tuning. If the patient feels a “burn” or a “single sting” under one electrode or the other, normally, this may be resolved by slightly increasing the intensity. If this procedure does not work, the electrode should be turned off and the electrode positioning should be changed. One should move the electrode slightly out of the pain area and resume the procedure. It is important to never keep active electrode pairs that do not produce the analgesic effect in the expected conditions. The patient can guide treatment to maximum intensity. The intensity should reach the maximum bearable without causing the patient to feel any significant discomfort. It is necessary to adjust the stimulation levels each time the patient experiences a decrease in stimulus intensity.
These conditions can be summarized by: the need for a
standard training training
courses , completion of learning curve, full
compliance to standard protocols diversified in chronic non-cancer
and cancer pain, correct management of incompatible drugs, and
self-assessment in the ability to correctly use the Scrambler
Therapy.
While performing clinical trials, the same team should be used that has successfully completed the learning curve required for proper use of the ST.
Like most clinical practice procedures, the device usage instructions do not replace an adequate course of training, which normally lasts for 3 days.
The key to the pain system remodulation process achieved by Scrambler Therapy is the ability to eliminate the pain (or at least get it to VAS < 2/10) during each treatment session, without the patient feeling any discomfort due to stimulation.
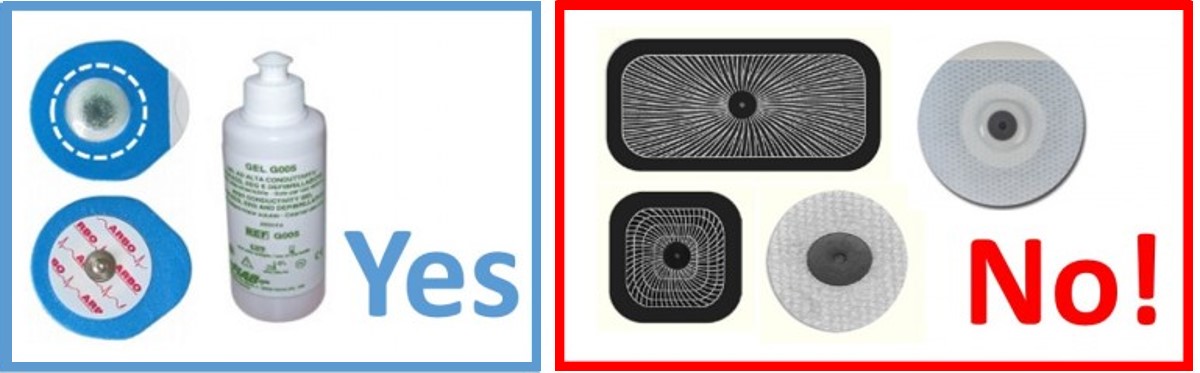
Optimally, EKG electrodes with spongy contact surfaces are recommended for use. The use of different electrodes may decrease the effectiveness of ST due to the distortion of information, which also renders the patient’s perception less comfortable and may prevent a successful fine-tuning of the electrode stimulation. It is especially not recommended to use “large” electrodes, like the ones usually used for TENS. In this case, apart from the problems previously listed, the broad electrode surface may stimulate incorrect areas because of poorly selective recruitment. This could lead to a pain increase during or after the treatment. In addition, the much lower than expected impedance of these electrodes may cause continual intervention of the protections. This tends to “cut” the output emissions, producing a distortion of the information. Electrodes should not be reused, as this may impair the ability of ST to transmit information and may cause skin irritation. A small amount of gel should be added to the center of the electrode to optimize conduction.
Contact Download Video Tutorial Delta Research & Development
Copyright © Delta Research & Development. All rights reserved